Other Cancers
There are multiple other cancers known to us, which occur at a lesser frequency. Virtually every organ in the body can be involved and affected by cancer. Examples are Renal cancer, Liver cancer, Gall-bladder cancer, Stomach cancer, Oesophageal cancer, Urinary bladder cancer, Soft tissue sarcomas, Bone cancers, etc.
Human Papilloma Virus Associated Cancers
This virus only infects humans and causes no harm to those with strong immunity. However, if immunity is weakened, the virus can lead to cancer and other infections.
Cancers of the head and neck
Cancer of the oral cavity, pharynx, larynx, tongue, and tonsils (head & neck) are often linked to HPV 16 and carry a better prognosis. HPV-linked cancers are less aggressive and respond better to treatment, making them easier to control.
Cervical Cancer
Cervical cancer is a common cancer in women, caused mainly by HPV infection. HPV types 16 and 18 account for 90% of cases. The HPV vaccine reduces the risk of developing cervical cancer. If detected early, it can be cured completely.
Anal cancer
A relatively rare malignancy, it is caused by HPV 16 & 18 in almost 90% of the patients.
Cancers of the Vulva, Vagina and Penis
Cancers of the vulva, vagina, and penis are rare cancers affecting the reproductive organs. Causes include genetics, lifestyle factors, and infections (e.g. HPV). Early detection is key, and regular cancer screenings can help diagnose these cancers early.
Genital and Nongenital Warts(Non-cancerous)
Genital warts are a type of sexually transmitted infection, genital warts are caused by HPV types 6 and 11. Sexual contact with an infected individual is believed to be the mode of spread. Nongenital warts are also caused by HPV, but are not typically associated with an increased risk of cancer.
Immunotherapy: Making Incurable Cancers into Chronic Diseases
- Immunotherapy: is the new kid on the block. It has revolutionised the treatment of multiple malignancies and has fostered a great deal of hope for the future. It is one of the few treatments that may eventually lead to a cure for conditions like Lung Cancer, a highly lethal illness which is incurable and eventually terminal.
- Immunotherapy functions in a novel manner to treat a cancer. It does not attack the cancer cells directly. It primes the patient’s immune system to attack the tumour cells. In simple terms, it awakens the body’s suppressed defence mechanism by breaking down the protective shield that the cancer cells use to protect themselves against attack. Once this shield is down, the immune system suddenly realises that there is a foreign object in the body which must be eliminated, it attacks the tumour and pushes the malignancy into remission.
- It is given intravenously as a 30-minute injection, administration is pain less and the drug is extremely well tolerated. Quality of life is maintained, there is generally no hair loss and the patient can resume work the very next day. Immune related side effects can occur in a few patients but these can be controlled with medication.


Understanding Melanoma - Skin Cancer
The three main types of skin cancer are Basal Cell Carcinoma, Squamous Cell Carcinoma, and Melanoma. Early detection is crucial for successful treatment and cure. Be mindful of changes in skin appearance and seek medical advice if needed.
Malignant Melanoma
- Melanoma is a type of skin cancer that is highly lethal, its incidence increases with age. The chance of a cure depends on early detection, a late-stage diagnosis is generally fatal.
- There are various types of melanoma, including cutaneous, uveal, and acral.
- It usually develops as a pigmented lesion over the skin or mucosa, which gradually increases in size, becomes invasive and results in metastasis.
- Risk factors include light skin, excessive sun exposure, UV light exposure, immunosuppression, PUVA therapy, and the presence of many common moles.
- Any pigmented lesion that suddenly begins increasing in size, shows asymmetry, has irregular borders, variation in colour, and a diameter greater than 6mm, must be investigated further.




Squamous Cell Carcinoma of Skin
- It is one of the cancerous lesions of the skin that develops from the epidermal keratinocytes. It is the second most common type of skin cancer.
- It can develop on any cutaneous surface like the head, neck, chest, back, arms, legs, oral mucosa, and genital area.
- Excessive sunlight exposure, exposure to ultraviolet light like tanning beds or the use of PUVA therapy, lighter complexion, older age, radiation treatment, smoking, and immunosuppression are all risk factors.
- It can be seen as a pigmented lesion, or a reddish, scaly patch. Invasive lesions can be seen as firm nodules, papules or plaques.
Basal Cell Carcinoma of Skin
- One of the common skin cancers, they are seen more frequently in men than women, with the incidence increasing with age. Lighter complexioned individuals are at a higher risk, the cancer is uncommon in darker skin.
- Exposure to ultraviolet radiation from the sun is a major risk factor. The use of tanning beds, therapeutic use of PUVA treatment, radiation therapy, chronic arsenic exposure from ingestion of contaminated food or water, inherited genetic mutations and immunosuppression due to cancer, HIV, organ transplant etc are the other risk factors.
- The face is the commonest site for the development of a basal cell carcinoma.
- A basal cell carcinoma can present as a pinkish or a flesh-coloured nodule on the face, on the trunk it can be seen as a light red or pink patch or plaque.
- Most of these cancers remain localised but a few can turn aggressive and metastasise. The stage at which it is diagnosed determines the treatment and the chances of a cure.


Skin Cancer Prevention


- Excessive ultraviolet light exposure through sun rays is a major cause of skin cancer. Minimize exposure by limiting time in the sun, especially during peak hours.
- Use protective clothing, such as hats, long-sleeved shirts and pants, and sunglasses. Apply sunscreen with an SPF of at least 15 or higher on all exposed areas of the skin. An SPF of 30 is recommended.
- Reducing or avoiding the use of tanning beds to get artificial tans is recommended to reduce the incidence of skin cancer from this source.
- Atypical nevi and a large number of common nevi, more than 50, are risk factors for melanoma. These skin conditions which resemble moles, must be monitored closely to detect any malignant transformation.
- Patients who are immunosuppressed, including HIV-positive patients, solid organ transplant recipients, and cancer patients receiving certain targeted therapies, are at a higher risk for skin cancer.
- These patients must undergo regular total skin examinations and be screened carefully for any pre-cancerous lesions. Any skin cancer lesion must be treated immediately if detected.
Skin Cancer Treatment
As per Type
The three principal skin cancers, Squamous cell carcinoma, Basal cell carcinoma, and Malignant Melanoma are all curable if detected in the initial stages before spread occurs. Treatment in the early stages involves surgery for all three types of skin cancers with or without radiation. Once the cancers become invasive and metastasise, surgery plays no role, and systemic treatment is required.


Localized Skin Cancer
When there is no distant spread, the skin cancer lesion should be surgically removed. If it is in an area that cannot be operated on safely, then curative radiation is an option.
Following surgery, if the lesions are large, or positive margins are seen on the final pathology, post operative radiation is given.
Very early stage skin cancers, either squamous or basal cell carcinoma can also be treated with cryotherapy, curettage & electrodessication, topical & intralesional therapies.
Areas like the head and neck, hands, feet and genitalia, when involved with a skin cancer, can undergo Mohs micrographic surgery instead of standard surgical excision. This is a more precise surgical procedure that allows removal of the entire lesion with good cosmetic results and minimal removal of normal tissue.
Patients who are not surgical candidates due to age, morbidity or the location of the lesion can receive curative radiation.
In malignant melanoma wide excision of the cancer along with lymph node evaluation and dissection is required in the non-metastatic lesions that can be completely excised. Such patients may require post-operative radiation and adjuvant treatment with Immunotherapy depending on the final histopathology report, the size of the lesion, extent of local spread, and number of lymph nodes involved.
Once the skin cancer becomes invasive and metastases develop, surgery and radiation are either not possible or are insufficient. Systemic therapy is then indicated using chemotherapy, Immunotherapy, and targeted therapy like the hedge-hog inhibitors.
Locally Advanced and Stage Four Skin Cancer
New data in locally advanced squamous cell skin cancer indicates that initial treatment with Immunotherapy followed by a complete surgery gives excellent results. It also reduced the surgical morbidity and improved the cosmetic outcome.
Patients with metastatic squamous cell carcinoma of skin who cannot be cured with surgery and radiation require systemic treatment for palliation and disease control.
Immunotherapy is the first option in all patients with locally advanced or metastatic squamous cell skin cancer who are ineligible for surgery/radiation. Either Pembrolizumab or Cemiplimab can be used, with both showing a good response and disease control. This treatment may also result in previously advanced lesions becoming resectable & thus offering hope for a cure.
Patients’ ineligible for Immunotherapy due to immunosuppression or an autoimmune disease, can be offered chemotherapy with Paclitaxel & Carboplatin or targeted therapy with Cetuximab, an EGFR inhibitor.
Patients with extensive or metastatic basal cell skin cancer who are not eligible for curative treatment with surgery or radiation may receive systemic treatment such as targeted therapy with Vismodegib or Sonidegib to block cancer cell proliferation and growth. Immunotherapy with Cemiplimab is a second line option, while Itraconazole, an antibiotic and a hedgehog pathway inhibitor, can be used if patients cannot receive or progress on immunotherapy. Chemotherapy with Paclitaxel and Carboplatin is another option for patients who do not respond to other treatments.
Locally Advanced & Metastatic Malignant Melanoma
All patients with advanced and metastatic melanoma must undergo a detailed molecular profiling of the tumour, to identify disease driving mutations that can be targeted. Treatment with Immunotherapy is the first option in these patients. Pembrolizumab or Nivolumab in combination with Ipilimumab is recommended. Nivolumab with Relatlimab is another emerging treatment option. Both these combinations provide effective cancer control and extend progression free & overall survival. Those who progress on Immunotherapy after a period of control can receive targeted therapy depending on the underlying mutations detected. About half of these patients will be carrying a BRAF V600 mutation. This mutation combines with MEK to stimulate the MAPK pathway, which in turn activates the cancer cells leading to spread. The use of a combined BRAF plus MEK inhibitor works effectively to block the cancer cell proliferation and suppress the tumour. The drugs used are Dabrafenib plus Trametinib, Vemurafenib plus Cobimetinib & Encorafenib plus Binimetinib. Those without the BRAF mutation must be evaluated for other actionable mutations by performing a molecular analysis of the cancer. Radiation can be given for symptomatic treatment like pain relief or local tumour control. Chemotherapy may be used in patients after all the above options are exhausted. Paclitaxel with Carboplatin, Dacarbazine and Temozolamide are the drugs that can be used.
Frequently Asked Questions For Skin Cancer
The presentation of skin cancer varies depending on the type of cancer and the area it develops in. it may be seen as a pigmented patch, an ulcerated area, a reddish or an erythematous patch. Nodules, papules, plaques can occur. Melanoma usually presents as a pigmented lesion.
Any unusual lesion on any region of the body must be investigated. Any sudden increase in the size of a skin lesion, a pigmented lesion that shows asymmetry, irregular borders, varied colour throughout the lesion, diameter more than 6mm, any recent change in the skin lesion or development of a new lesion, any skin lesion that looks different from other surrounding lesions, all these signs must be promptly investigated.
In the initial stages, skin cancers remain asymptomatic. It is only when they become invasive and increase in size do they produce symptoms like pain and ulceration. Symptoms in advanced skin cancer will depend on the region involved. There may be itching and redness related to the lesions. Lymph node swellings may also occur in the region around the skin cancer.
Any unusual skin lesion which has suddenly developed, any long standing pigmented lesion which has suddenly started increasing in size, shows asymmetry, irregular borders, changes in colour of the lesion, lymph node swellings in the region of the skin lesion can all be signs of skin cancer.
Other skin lesions, like an inflammatory lesion- psoriasis, eczema, seborrheic keratoses can be mistaken for skin cancer. Dermal nevi, keratoacanthomas, actinic keratoses, melanocytic nevus, lentigo; are some other conditions that resemble skin cancer.
Early signs of skin cancer can include new moles or changes in existing moles, dark, scaly patches on the skin, rough, scaly patches that won’t heal, raised, red, pearly bumps, and dark, bleeding sores that won’t heal. It’s important to check your skin regularly and see a doctor if you notice any changes.
Malignant melanoma, Squamous cell carcinoma and Basal cell carcinoma are the commonest type of skin cancers.
Melanoma skin cancer can prove fatal if not diagnosed early and treated immediately.
Skin lesions of melanoma usually appear as a pigmented patch, a pigmented nodule or area initially.
Yes, if detected early & treated appropriately, melanoma can be cured.
Thyroid Cancer Symptoms & Signs
- Thyroid cancer may not cause any symptoms in its early stages.
- The typical presentation of a thyroid cancer is in the form of a thyroid nodule. Initially it may remain extremely small, increasing in size as the cancer cells proliferate.
- The nodule may be seen or felt by the patient, detected during a physical examination, or seen incidentally during an imaging study, like a neck CT or Sonography.
- A rapid growth of a malignant nodule may occur, with invasion into the adjacent tissues-the nodule may become fixed to the surrounding structures with cancer progression.
- Other symptoms, like a sudden onset hoarseness of voice, difficulty in swallowing, a unilateral vocal cord paralysis, & development of a neck swelling on one side due to the cancer spreading into the cervical lymph nodes can all be seen as the thyroid cancer progresses.
- A thyroid mass can be seen in the neck, as the cancer increases in size. Symptoms due to compression of the surrounding structures like hoarseness and dysphagia can then occur.
- A rapidly growing mass can cause pain and tenderness in the neck. Compression of the trachea by the cancer can cause cough & breathlessness. With spread into the lungs, bones and other organs, loss of appetite, weight loss, weakness, chest pain, abdominal pain , headache & confusion can all develop.


Types of Thyroid Cancer
Undifferentiated thyroid cancer-known as Anaplastic cancer. It is an extremely aggressive cancer, fast spreading, usually detected in the advanced stages and generally proving fatal.
The well differentiated thyroid cancers- Papillary and Follicular cancers. Papillary cancers are the commonest type of thyroid cancer detected. They are slow growing, amenable to treatment & carry a good prognosis.
Neuroendocrine thyroid cancer-known as Medullary cancer. It may be sporadic or occur as a part of the MEN syndrome. If detected in the early stages it can be cured.
Follicular cancer, another type of well differentiated thyroid cancer, it occurs in a lesser frequency than the papillary cancers. It is usually diagnosed early and carries a good prognosis. Hurthle cell cancer is one of its variants.
Thyroid Cancer Treatment
- The initial treatment for all types of thyroid cancer is a complete surgical resection. The only time systemic treatment is indicated upfront is if the cancer has already spread, is metastatic & inoperable.
- At all other times an initial surgery is performed. The surgical options are a total or a near total thyroidectomy or a unilateral lobectomy with isthmusectomy. The surgical procedure choice depends on the initial stage and extent of the cancer, size of the primary tumour, the presence of spread outside the thyroid, whether lymph node metastases has occurred, age of the patient, physical condition & presence of any comorbidities.
- Following surgery, post operative thyroid hormone replacement is required in all patients.
- In well differentiated thyroid cancers, primarily Papillary & Follicular cancers, patients are risk stratified according to the stage of the cancer and its features.
- Low risk patients where the cancer is confined to within the thyroid do not require any further treatment.
- Postoperative Radio-iodine therapy is indicated in intermediate risk patients (presence of vascular invasion, lymph node metastases, aggressive histologies like tall cell, columnar or poorly differentiated cancers).
- It is also required in all high risk patients (presence of metastases, locally advanced cancers, incomplete tumour resection, presence of gross residual disease).
- This therapy is given to eliminate residual & metastatic cancer deposits and to treat micro metastatic cancer.
- External beam radiation is an option for the patients who do not respond to, or are unable to receive the radioiodine therapy.
Anaplastic Thyroid Cancer
- Patients who can undergo a complete surgical resection must receive post-operative radiation along with chemotherapy.
- Drugs recommended are Doxorubicin with Cisplatin, Doxorubicin alone or Docetaxel alone.
Medullary Thyroid Cancer
- Patients post a complete surgical resection do not require any further radiation. Radiotherapy however may be given for a residual or recurrent disease.
Metastatic Thyroid Cancer
- Patients with stage 4 thyroid cancer can undergo a palliative thyroid resection if indicated, to relieve pressure symptoms and pain.
These patients cannot be cured. - Their cancer can however be controlled with systemic treatment using targeted therapy with or without chemotherapy.
- Papillary & Follicular cancers can be treated with Radioiodine therapy if the metastatic deposits show radioiodine uptake. Patients post radioiodine therapy & those who cannot receive the therapy, both can receive treatment with targeted therapy in the form of oral tyrosine kinase inhibitors.
Is Thyroid Cancer Curable?
- Yes, thyroid cancer is often curable, especially if it is detected and treated in its early stages. The success of treatment for thyroid cancer depends on various factors such as the type and stage of the cancer, the age and overall health of the patient, and the specific treatment approach used.
- The most common treatments for thyroid cancer include surgery to remove the thyroid gland, radioactive iodine therapy, and thyroid hormone therapy. In some cases, external beam radiation therapy or chemotherapy may also be used. In many cases, a combination of these treatments is used for the best outcome.
- It’s important to note that every case of thyroid cancer is unique and the prognosis can vary widely. If you have been diagnosed with thyroid cancer, it’s important to work closely with your healthcare team to determine the best treatment plan for you.
- Papillary and Follicular cancers can be treated with Radioiodine therapy if the metastatic deposits show radioiodine uptake.
- If not, patients can receive targeted therapy in the form of oral tyrosine kinase inhibitors.
- Molecular profiling of the tumor is performed to detect targetable mutations, and therapy is directed toward these mutations if detected.
- If there are no targetable mutations, patients can receive Lenvatinib in the first line and Sorafenib in the second line.
- Chemotherapy with Doxorubicin can be used as a last resort. Targeted therapy is effective in controlling and stabilizing the disease.
Anaplastic Thyroid Cancer
- All patients with an anaplastic cancer must undergo a detailed molecular profiling to detect targetable mutations. BRAF V600E mutation can be detected in a large number of these patients.
- They can receive oral treatment with tablets Dabrafenib & Trametinib.
- Those who test negative for BRAF, may carry other mutations like RET,TRK,ALK,TSC1 & TSC2.
- Mutation directed therapy can then be given.
- Chemotherapy using Doxorubicin alone or in combination with Cisplatin, or Paclitaxel as a single agent are other options to consider after loss of response to targeted therapy.
Medullary Thyroid Cancer
- A detailed molecular profiling is also indicated in these patients. Again, mutation directed therapy is the best option.
- RET mutated cancers can be treated with targeted therapy- Selpercatinib or Pralsetinib.
- Those patients with no detectable mutations can receive oral therapy with Lenvatinib, Cabozantinib, Vandetanib, Sorafenib or Sunitinib.
- All these drugs work to stabilize and control the cancer and reduce the speed of progression.
- They provide effective palliation of symptoms.
- External beam radiation can also be used for palliation to control pain or local symptoms.
- Chemotherapy is an option following targeted therapy.
- Dacarbazine in combination with Cyclophosphamide & Vincristine is the recommended regimen. However, efficacy is less than seen with targeted therapy.
Our Survival Stories
Frequently Asked Questions For Thyroid Cancer
Yes, if detected early, thyroid cancer can be completely cured.
There are multiple causes of thyroid cancer. In many patients the precise cause cannot be determined. Radiation exposure during childhood, as in environmental exposure or radiation to the neck during childhood increases the risk for development of thyroid cancer in future life. Some patients may be carrying underlying mutations that predispose them to thyroid cancer occurrence. A positive family history, especially in a first degree relative, of thyroid cancer or a thyroid cancer syndrome is a risk factor.
Any swelling, mass or nodule in the neck is usually the first sign of a thyroid cancer. It must be investigated immediately. Sudden onset hoarseness of voice, dysphagia, a long standing nodule suddenly increasing in size, must all raise a red flag and be evaluated.
A large swelling in the neck that is fixed to the underlying structures, hoarseness of voice, cough, breathlessness, difficulty in swallowing, neck pain, tenderness, increasing size of neck swelling, all indicate that the thyroid cancer is spreading.
In the initial stages thyroid cancer remains asymptomatic. It normally presents as a nodule in the neck, in the thyroid gland. As it increases in size, a mass or swelling can be seen and felt in the neck. With progression, it can cause pressure symptoms like difficulty in swallowing, hoarseness of voice, cough, swellings on both sides in the neck as the cervical lymph nodes are involved by the cancer.
A thyroid cancer when suspected, requires a neck sonography to evaluate the thyroid nodule or mass, followed by an FNAC to check for presence of cancer.
Thyroid cancer is caused by abnormal growth and division of cells in the thyroid gland, with risk factors including radiation exposure, genetic mutations, family history, medical conditions such as goiter, and environmental factors like tobacco smoke and air pollution. The exact cause is unknown.
It is difficult to prevent thyroid cancer from developing, but a regular physical examination and neck sonography will ensure that it is diagnosed in the early stages.
If detected in the early stage, thyroid cancer can be cured completely, ensuring extremely high survival rates.
You can examine your neck with your hands, to check for any swelling or mass. A visual inspection in the mirror can be done of the neck. The best test would be to do a sonography of the neck, to evaluate the thyroid gland.
Oesophageal Cancer Symptoms & Signs
- Difficulty in swallowing or dysphagia is usually the first sign of an oesophageal cancer.
- Initially the dysphagia is for solids, followed by liquids, as the cancer increases in size and blocks the lumen of the food pipe or oesophagus.
- As a result, collection of food that is eaten occurs in the food pipe, as passage into the stomach is obstructed.
- Nausea and vomiting occurring immediately or a few hours following food intake is seen.
- This is followed by weight loss, weakness, fatigue and a loss of appetite as the cancer spreads and nutrition is impaired.
- Bleeding from the cancer can result in blood-stained vomiting, loss of a large quantity of blood with vomiting or haematemesis, loss of blood in the stools or melaena (passage of black coloured stools).
- The blood loss results in anaemia and a drop in hemoglobin. Painful swallowing or odynophagia can occur.
- As the cancer spreads, systemic symptoms develop. Lung involvement can cause cough & breathlessness with chest pain.
- Bone metastases can cause pain. Liver metastases causes jaundice, ascites, low albumin and clotting disorders.
Oesophageal Cancer Treatment
- Oesophageal cancer is an extremely aggressive cancer that spreads quickly.
- It is generally detected when extensive metastases have already occurred & the patient is symptomatic.
- The 2 main pathologies seen are Adenocarcinoma & Squamous Cell Carcinoma.
Early stage Oesophageal Cancer
This refers to oesophageal cancer that is localised within the epithelium and invasion into and beyond the muscle layer has not occurred. The depth of penetration determines the treatment. Extremely small areas of cancer, which only involve the superficial layer can be treated by endoscopic resection alone. Deeper penetration into the submucosa requires a radical surgery/ Esophagectomy. Patients unfit for a surgery can receive radical, curative, combination or concurrent chemotherapy plus radiation. Low dose weekly Paclitaxel & Carboplatin are given with radiation. Such patients have a good chance of a cure.
Locally advanced Oesophageal cancer
Oesophageal cancer that has spread into the muscle layer of the oesophagus & beyond, has invaded the surrounding tissues of the oesophagus or has spread into the regional draining lymph nodes is known as a locally advanced cancer.
Such patients must not undergo surgery upfront. They require neoadjuvant (preoperative) therapy in the form of concurrent CT RT (chemotherapy plus radiation administered simultaneously). Along with daily radiation, weekly low dose chemotherapy with Paclitaxel & Carboplatin is given. This treatment helps to down size the cancer and eradicate microscopic cancer cells in the blood stream that can result in metastases.
Post CT RT a radical surgery/Esophagectomy is performed. Any viable cancer cells detected in the histopathology specimen post operatively are treated with a course of IMMUNOTHERAPY or chemotherapy, using drugs the patient has not been exposed to. (If Immunotherapy cannot be given).
Locally advanced cancer that has been operated without neoadjuvant CT RT, must receive adjuvant, post operative treatment with chemotherapy followed by concurrent CT RT.
Stage 4 Oesophageal cancer
This refers to oesophageal cancer that has metastasised or spread extensively. Bones, lungs, liver, brain can all be involved with the cancer. In this stage a cure is not possible & treatment becomes palliative.
A detailed molecular profiling of the tumour by performing next generation sequencing is essential. This enables detection of any disease-causing mutations that can be targeted. Immunotherapy markers must be analysed as well. A combination of targeted therapy plus chemotherapy is more effective in obtaining disease control, than chemotherapy alone.
Markers that must be analysed before commencing treatment are HER2, MSI status, PD-L1 level, TPS/CPS score.
Oesophageal Adenocarcinoma
Between 7% to about 35% of adenocarcinomas will show HER2 overamplification. These patients must receive treatment with a combination of targeted therapy (Trastuzumab) with chemotherapy. Immunotherapy must be added to this regimen. The protocol should comprise Trastuzumab, Pembrolizumab (Immunotherapy) added to the FOLFOX regimen.
Adenocarcinomas that show no HER2 overexpression, but show elevated levels of PD-L1, must receive Nivolumab, the immunotherapy drug, in combination with chemotherapy (FOLFOX or CAPOX) regimen.
Patients with low levels of PD-L1 must receive chemotherapy alone.
Patients with deficient mismatch repair or microsatellite high/unstable tumours (dMMR/MSI) can receive immunotherapy alone or in combination with chemotherapy. This is applicable to both adenocarcinomas & squamous cell carcinomas.
FOLFOX is the chemotherapy regimen recommended as first line therapy either alone or in combination with targeted therapy or immunotherapy.
Squamous cell carcinoma
Oesophageal squamous cell carcinomas with high levels of PD-L1 must receive chemotherapy with immunotherapy in the first line. Cancers who show low levels of PD-L1 also show some degree of benefit with immunotherapy & this must be added to chemotherapy. Pembrolizumab or Nivolumab can be added to the FOLFOX regimen.
Besides the above guidelines, treatment can be tailored as per the molecular profiling & underlying mutations detected.
There are a number of chemotherapy regimens that can be used in the second line, following progression on FOLFOX. Docetaxel, Irinotecan, Cisplatin, Paclitaxel & Epirubicin can all be used in various combinations.
FLOT regimen, modified DCF/TCF, CAPOX, FOLFIRI are the other second and third line regimens that can be used.
Frequently Asked Questions For Oesophageal Cancer
Without treatment it is not possible to live for a long time with oesophageal cancer, as it is eventually a terminal illness.
Oesophageal cancer in very early stages has good cure rates.
Smoking & alcohol consumption are major risk factors for oesophageal cancer.
Upper GI Endoscopy to visualise the oesophagus followed by a biopsy of any suspicious lesion is the procedure required to diagnose oesophageal cancer.
Yes, without appropriate treatment, oesophageal cancer spreads rapidly.
Although usually seen in older age, in the presence of risk factors like smoking & alcohol, it can develop at any age.
In the final stages, there would be extensive spread of the cancer with involvement of the liver, lungs, bones & brain. The patient would be very weak and probably bedridden due to poor oral intake.
If detected in the initial stages radical CT RT, which means- a combination of chemotherapy & radiation administered simultaneously or concurrently, can be given to cure the cancer without surgery.
The treatment for oesophageal cancer depends on the stage at which it is detected. In stage 4 cancer, a combination of chemotherapy, immunotherapy and targeted therapy is the best treatment. Surgery, radiation and chemotherapy are used when the cancer is locally advanced.
When the patient complains of difficulty in swallowing, which is increasing gradually, this should be investigated immediately with an endoscopy, to look for oesophageal cancer. A biopsy of any suspicious lesion is needed to confirm the diagnosis.
Early detection is key, book an oesophageal cancer screening now to protect your future
Stomach Cancer Causes
- Infection with the Helicobacter Pylori or H.pylori organism is one of the chief causes of gastric or stomach cancer. The inflammation in the stomach triggered by H.pylori results in continuous irritation within the stomach tissues resulting in atrophy & metaplasia which eventually progresses to a cancer.
- High salt intake and salt-based methods of preservation of food are believed to be linked to stomach. Consumption of salted meat, salted fish etc. all increase the risk.
- Exposure to N-nitroso compounds in the diet, from tobacco smoke, environment, other food sources can result in stomach cancer.
- Consumption of processed meat is linked to a high risk of stomach cancer formation.
- Obesity has been correlated with an increase in risk of stomach cancer.
- Tobacco consumption, smoking, alcohol intake, are all associated with a high risk of occurrence of stomach cancer.
- Epstein-Barr virus infection can trigger the development of stomach cancer.
- Patients who have received abdominal radiation for treatment of other cancers are at an increased risk.
- Approximately 3% of stomach cancers are hereditary, they can cluster within families and are linked to gastric cancer syndromes like Hereditary Diffuse Gastric Cancer.
- Pernicious Anaemia is associated with a high risk of gastric cancer.
Stomach Cancer Treatment
Cancers that involve the oesophagogastric junction or the gastric cardia, with cancer extending up to 2cm into the proximal stomach, are treated on the same treatment lines as Oesophageal Cancer. The same treatment protocols are followed, the same chemotherapy drugs and immunotherapy regimens are used.
Early gastric cancer:
Refers to invasive gastric cancer that involves the mucosa or submucosa of the stomach, but does not invade beyond. Draining lymph nodes may or may not be involved.
If H.pylori infection is detected, this should be treated & eradicated with antibiotic therapy. This can prevent precancerous lesions from progressing to cancer. It can also prevent the development of a second gastric cancer after treatment for early stomach cancer.
Patients found to have lymph nodes involved with cancer, must undergo complete surgery or a gastrectomy.
Those without lymph node involvement, having a tumor less than 20mm, which is well differentiated on biopsy, without ulceration or lymphovascular invasion, can undergo an endoscopic resection of cancer. If this procedure cannot remove the entire cancer, then complete surgery is necessary.
All cancers with positive lymph nodes must receive adjuvant chemotherapy post-surgery.
Stomach cancer that extends beyond the submucosa (all lesions T2 and higher) and locally advanced cancers:
This applies to the stomach cancers that originate beyond the initial 2cm of the stomach. (non cardia gastric cancer).
For all these patients, initial, preoperative chemotherapy is required. This plays a crucial role in down sizing the cancer & eliminating any microscopic cancer cells in the blood stream. This should then be followed by a complete, radical surgery to remove all gross tumour.
Chemotherapy regimens recommended are FLOT followed by FOLFOX, for those who may not tolerate FLOT.
Patients who have already undergone an initial surgery must receive post operative chemotherapy followed by chemoradiotherapy, in the event of positive lymph nodes, an incomplete surgery (less than 16 lymph nodes examined) or presence of cancer that could not be completely removed.
Those who have had a complete surgery with no lymph node involvement can receive post operative chemotherapy alone.
Oral capecitabine can be combined with radiation.
FLOT or FOLFOX are the chemotherapy regimens to be used.
All gastric cancer patients must undergo a detailed molecular profiling at diagnosis, before treatment initiation, to look for potentially targetable mutations and markers indicating benefit from immunotherapy.
MSS/MSI status or dMMR must be assessed as well. Those with a Microsatellite high or unstable or a mismatch repair deficiency will benefit from immunotherapy. Such patients may not require additional chemotherapy.
Advanced or metastatic stomach cancers:
This refers to the stomach cancers that show extensive spread with involvement of multiple organs like the liver, lungs, bones & brain.
This is a stage 4 cancer. In this stage, the stomach cancer cannot be cured, it can be controlled using a combination of chemotherapy, targeted therapy & immunotherapy. Treatment intent is palliative. It works to improve & maintain the quality of life, and give patients a longer progression free survival from the cancer.
A detailed molecular profiling of the tumour by performing next generation sequencing is essential. This enables detection of any disease-causing mutations that can be targeted. Immunotherapy markers must be analysed as well. A combination of targeted therapy, immunotherapy plus chemotherapy is more effective in obtaining disease control, than chemotherapy alone.
Markers that must be analysed before commencing treatment are HER2, MSI status, PD-L1 level, TPS/CPS score.
Majority of the stomach cancers detected are adenocarcinomas.
Some percentage of the gastric adenocarcinomas will show HER2 overamplification. These patients must receive treatment with a combination of targeted therapy (Trastuzumab) with chemotherapy. Immunotherapy must be added to this regimen. The protocol should comprise Trastuzumab, Pembrolizumab (Immunotherapy) added to the FOLFOX regimen.
Adenocarcinomas that show no HER2 overexpression, but show elevated levels of PD-L1, must receive Nivolumab, the immunotherapy drug, in combination with chemotherapy (FOLFOX or CAPOX) regimen.
Two immunotherapy drugs- Nivolumab plus Ipilimumab is another option.
Patients with low levels of PD-L1 must receive chemotherapy alone.
Patients with deficient mismatch repair or microsatellite high/unstable tumours (dMMR/MSI) can receive immunotherapy alone or in combination with chemotherapy.
FOLFOX is the chemotherapy regimen recommended as first line therapy either alone or in combination with targeted therapy or immunotherapy.
Other regimens that can be used in the second and subsequent lines are FLOT, TCF, DCF, CAPEOX, Docetaxel plus S1, Docetaxel plus Cisplatin, and Irinotecan based regimens.
Besides the above guidelines, treatment can be tailored as per the molecular profiling & underlying mutations detected.
Frequently Asked Questions For Stomach Cancer
Any unexplained loss of appetite, followed by loss of weight, weakness, early satiety, and fatigue, associated with gradual onset abdominal pain, which continues to increase in intensity can all be warning signs for stomach cancer. Nausea & vomiting may be present in the initial or later stages of the cancer.
If detected in the early stage, stomach cancer can be cured.
Life expectancy depends on the stage the stomach cancer is detected in. Detection in the early stages ensures a good life expectancy. If diagnosed in the advanced stages, the cancer is terminal.
Cancer of the stomach is an extremely lethal disease; it can prove fatal if not treated immediately. It is highly aggressive and spreads rapidly without timely treatment.
An upper GI Endoscopy is required to visualize the stomach, followed by a biopsy of any suspicious lesions seen. This will give the diagnosis of stomach cancer if present.
Processed meat, processed fish, a high intake of salt, salt-based methods of food preservation all increase the risk of stomach cancer. Consuming salted meats is linked with stomach cancer.
A person who consumes large quantities of alcohol, a chronic smoker or tobacco chewer, an obese individual, a person who has received abdominal radiation, an individual with a family history of stomach cancer, are all at a risk for stomach cancer.
No, stomach cancer is not triggered by stress.
Stomach cancer treatment in India is affordable and equivalent to treatment given abroad. The cost of therapy in India is lower than in most other countries, with the same medications being utilised. The precise cost depends on the stage the cancer is detected in and the treatment required.
If detected in the early stages, the success rate in treating the stomach cancer is high. The cancer can be cured in these circumstances.
Take the first step towards early detection and prevention, schedule a stomach cancer screening with us today
Pancreatic Cancer Causes


Cigarette smoking & tobacco consumption are major risk factors for pancreatic cancer.


Heavy alcohol consumption is another major risk factor.


Obesity and a lack of physical activity increases the risk.


A diet high in saturated fat, processed or smoked meat, are all linked to pancreatic cancer.
Infection with H.pylori organism is associated with pancreatic cancer development.
Some clinical trials indicate an association between pancreatic cancer and Hepatitis B or C infection.




Emerging data indicates an association between diabetes mellitus, abnormal glucose metabolism, insulin resistance and development of pancreatic cancer.


About 5% to 10% of pancreatic cancers have a hereditary association. A family history of pancreatic cancer is a risk factor for the disease. Inherited mutations like BRCA, ATM, PALB2, CDKN2A & MLH1 are all predisposing factors for pancreatic cancer. These are deleterious, germline mutations which are passed on from one generation to the next.




Cystic fibrosis patients are associated with a high risk of pancreatic cancer.




Chronic pancreatic inflammation, as seen in chronic pancreatitis increases risk for pancreatic cancer.
Symptoms of Pancreatic Cancer
- Loss of appetite followed by weight loss; fatigue & weakness are the usual presenting symptoms.
- This is followed by abdominal pain, initially mild in intensity, and then gradually increasing to become severe. It arises in the epigastric region with radiation to the sides or the back. It is initially intermittent, later becoming continuous. Eating or lying down aggravates the pain.
- Severe back pain not responding to symptomatic treatment must arouse suspicion for a pancreatic cancer (usually in the body or tail of the pancreas).
- Sudden onset jaundice can be an early sign of a pancreatic cancer arising in the head of the pancreas. It can be accompanied by generalised itching, dark coloured urine & yellowish discolouration of the eyes.
- A recent onset of Diabetes Mellitus may be seen. Any sudden rise in sugars, or a new diagnosis of Diabetes Mellitus must prompt an investigation for pancreatic cancer.
- Unexplained thrombo-embolic episodes can occur due to the hypercoagulable state present in pancreatic cancer. Blood clots can suddenly develop in arteries or veins. Example, lower limb venous thrombosis.
- Depending on the extent of spread, signs of metastatic disease may be seen. For Example jaundice, ascites, an abdominal mass that can be felt, cough & breathlessness due to lung metastases, left supraclavicular lymph nodes due to involvement by the cancer, skin lesions like bullous pemphigoid, pain from the cancer or the metastasis can occur.
- Very rarely, pancreatic cancer may be detected incidentally, on imaging done for another condition.
Pancreatic Cancer Treatment
A PET-CT Scan must be performed in all pancreatic cancer patients as a metastatic work-up, to assess the extent of disease.
A detailed molecular profiling must be performed of all pancreatic cancers to look for mutations that can be targeted and to check for HRR (Homologous Recombination Repair) pathway deficiency.
Genetic testing of the patient is also necessary to check for inherited, cancer causing mutations that may have resulted in the pancreatic cancer development.
Mutations to look for with molecular profiling & genetic testing are BRCA1, BRCA2, PALB2, ATM, ATR, CHEK2, RAD51, & the FANC genes.
Pancreatic cancer that is localised within the pancreas, with no vascular invasion or metastasis, and is resectable:
- Such cancers should ideally receive pre-operative therapy. Three months of chemotherapy should be given. Following this, chemoradiotherapy is an option to consolidate the response.
- A complete surgical resection- Pancreatectomy with dissection of the draining lymph nodes must be performed.
- Post operative, 3 more months of chemotherapy must be given using the same pre-operative regimen.
- Pre and post-operative chemotherapy ensure eradication of the micrometastases, which are present in all pancreatic cancer patients, within the blood stream.
- All pancreatic cancer patients, even when extremely small & in the initial stages, must receive chemotherapy.
Locally Advanced or Borderline Resectable Pancreatic Cancer Patients:
- This refers to pancreatic cancer that is not resectable due to the spread of cancer in the tissues & lymph nodes around the pancreas, with vascular invasion.
- However, metastases to distant organs are absent. Following upfront chemotherapy, such patients may have a down-staging of their cancer sufficient to undergo a complete, radical surgery.
- These patients must receive initial chemotherapy followed by a reassessment for surgery. PET-CT Scans must be performed pre and post-chemotherapy.
- If surgery is not possible after the initial therapy, then chemotherapy must be continued. Chemoradiotherapy may be added to consolidate the response.
Upfront surgery:
- Pancreatic cancer patients who may have already undergone an upfront surgery without receiving any neoadjuvant or preoperative therapy must receive 6 months of adjuvant chemotherapy, irrespective of the stage of pancreatic cancer.
Maintenance therapy:
- Following completion of all treatment, patients detected with HRR pathway deficiency, due to the presence of mutations like BRCA or PALB2, can receive maintenance therapy with PARP inhibitors.
- Tab Olaparib or Rucaparib can be initiated and continued.
Chemotherapy regimens used in resectable, locally advanced, borderline resectable & unresectable pancreatic cancer:
- FOLFIRINOX or modified FOLFIRINOX is the regimen of choice as first-line therapy in young, physically fit adults. FOLFOX is an option for those who find FOLFIRINOX too toxic.
- In older adults, or those patients who are not physically fit, can receive Gemcitabine plus NabPaclitaxel, Gemcitabine plus Capecitabine or Gemcitabine plus S1.
- Radiation can be combined with oral Capecitabine or intravenous Gemcitabine.
Stage 4 or Metastatic Pancreatic Cancer :
The majority of pancreatic cancer patients are diagnosed in this stage. These patients are inoperable. Chemotherapy, targeted therapy, and Immunotherapy can be given singly or in combination for disease control. The aim of the treatment is palliation, pain control and improving and maintaining the quality of life.
All patients must undergo detailed molecular profiling by performing next-generation sequencing on the tumor sample. This enables the detection of underlying mutations that can be targeted. HRR pathway deficiency must be assessed.
A genetic testing of the patient must be performed to look for hereditary, high-risk, cancer-causing mutations that can be targeted.
Mutations to look for with molecular profiling & genetic testing are BRCA1, BRCA2, PALB2, ATM, ATR, CHEK2, RAD51, & the FANC genes.
- Above mutations can be targeted using the PARP Inhibitors– Olaparib & Rucaparib.
- Such cancers also respond well to the platinums, Cisplatin, Carboplatin & Oxaliplatin.
- MSS/MSI status must be assessed. If found to be microsatellite unstable, then Immunotherapy treatment can be given for the pancreatic cancer.
- Other markers for Immunotherapy must be tested on molecular profiling of the cancer.
- A high tumour mutation burden also indicates response to Immunotherapy. Pembrolizumab or Nivolumab are the drugs that can be used.
Other mutations if detected on molecular profiling that can be targeted are:
- RET fusion-positive cancers can be treated with Selpercatinib.
- TRK Fusion-positive cancers can be treated with larotrectinib or Entrectinib.
- RAS G12C mutated cancers can be treated with Sotorasib.
Chemotherapy regimens that are used are:
- FOLFIRINOX or modified FOLFIRINOX is the regimen of choice as first line therapy in young, physically fit adults. FOLFOX is an option for those who find FOLFIRINOX too toxic.
- In older adults, or those patients who are not physically fit, can receive Gemcitabine plus NabPaclitaxel, Gemcitabine plus Capecitabine or Gemcitabine plus S1. This can be given as first line therapy or as second line therapy after FOLFIRINOX or FOLFOX.
- Radiation can be combined with oral Capecitabine or intravenous Gemcitabine.
Other regimens that can be used after progression on the above drugs are those using Irinotecan. Single agent Gemcitabine or Capecitabine is an option in patients with a poor performance status.
Frequently Asked Questions For Pancreatic Cancer
Life expectancy post a diagnosis of pancreatic cancer depends on the stage it is detected in, in the advanced stages, the cancer is terminal, in the initial stages possibility of a cure exists with appropriate treatment.
Alcohol, smoking, tobacco consumption, nicotine exposure, are all considered the prime causes of pancreatic cancer.
Abdominal pain, initially mild, gradually increasing in intensity, mainly in epigastric region-radiating to sides and back, loss of appetite, weight loss, fatigue, weakness, feeling of indigestion are all signs of pancreatic problems.
Pancreatic cancer may be asymptomatic in the early stage. Abdominal pain, loss of appetite, weight loss, fatigue, weakness all develop as the cancer progresses.
Loss of appetite, weight loss, abdominal pain radiating to the sides & back and increasing in intensity & jaundice are the major symptoms.
If detected in the initial stage, before the cancer has spread or grown large, a cure is possible with appropriate treatment.
Maintaining a healthy life-style, avoiding alcohol, tobacco, smoking, exercising regularly, doing a regular health check-up, investigating any complaints like abdominal pain, loss of appetite and weight loss are some of the ways to avoid pancreatic cancer or diagnose it early.
Once pancreatic cancer spreads, life span is limited. The cancer spreads rapidly and usually proves fatal within 6 to 12 months. Appropriate treatment may be able to prolong life by about 12 to 18 months.
Pancreatic cancer is an extremely aggressive and fast spreading cancer. Without treatment it spreads quickly to multiple organs within a few months.
Follow the footsteps of renowned oncologist Dr. Sujata Vasani, prioritize your health and overcome the challenges of pancreatic cancer
Liver Cancer Types
Liver cancer can be a primary cancer, meaning it originates within the liver itself.
Hepatocellular carcinoma is the commonest primary liver cancer. It arises within the background of damaged liver parenchyma, underlying liver dysfunction & liver cirrhosis.
Other cancers that can originate within the liver are lymphomas & neuroendocrine tumours.
More commonly what is seen are liver secondaries, meaning spread of a cancer to the liver from a primary elsewhere in the body. Virtually any cancer can spread to the liver. Metastases are commonly seen from breast, lung, colon, rectal and ovarian cancers.
Liver Cancer Stages
- Staging is considered for primary Hepatocellular Carcinoma, which originates within the liver.
- The cancer may be localised within one lobe of the liver, small in size, with no spread within or outside the liver and no vascular invasion.
- Size is less than 2cm or between 2cm to 5cm in size.
- A large tumour or multiple tumours may be seen within one lobe of the liver with no spread outside the liver. Size may be more than 5cm.
- Multiple tumours may be seen involving both lobes of the liver with or without vascular invasion.
- Single tumour or multiple lesions with vascular invasion or direct spread into adjacent organs with deposits in the peritoneum and abdomen may be seen.
- In the advanced stages metastases to other organs and spread into regional lymph nodes is seen.
Causes of Hepatocellular Carcinoma
- Chronic liver disease, especially cirrhosis, is the primary cause of liver cancer.
- Hepatitis B and C infections can cause liver damage, cirrhosis, and cancer.
- Heavy and continuous alcohol intake is a major risk factor for cirrhosis and liver cancer.
- Any condition that causes cirrhosis is a risk factor for liver cancer.
- Tobacco intake can increase the risk of hepatocellular cancer.
- Intake of Aflatoxin B1, a food contaminant that can contaminate grains like corn, is a risk factor for liver cancer.
- Betel nut intake or chewing is a risk factor for liver cancer.
- Inherited disorders such as Hereditary Hemochromatosis, Alpha-1 antitrypsin deficiency, and acute intermittent porphyria increase the risk of liver cancer.
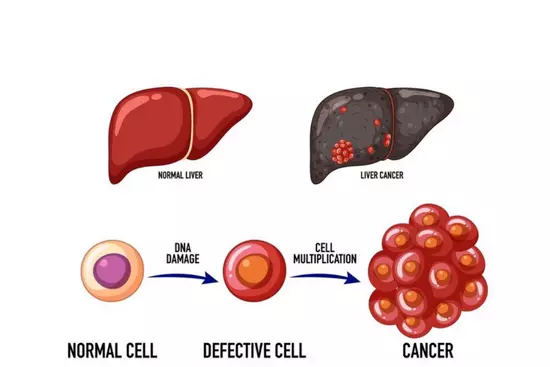
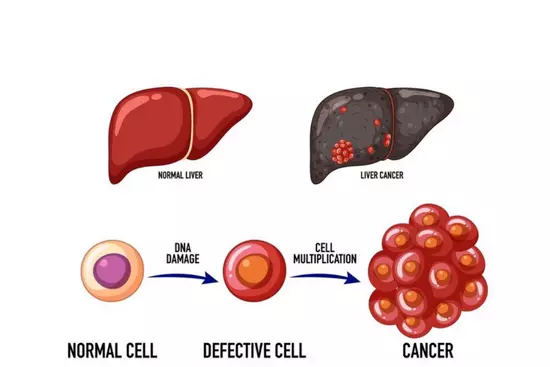
Process Of cancer development
Liver Cancer Diagnosis:
- It may be made incidentally when a liver lesion is seen on a sonography done as a part of a routine follow-up for a cirrhotic patient.
- Or it may be suspected due to symptoms like weakness, weight loss, abdominal pain, and jaundice.
- An elevated alpha feto-protein level , especially if greater than 400ng/ml, also points to the diagnosis of liver cancer.
- To confirm the diagnosis, a dynamic contrast enhanced CT Scan or MRI of the liver can be performed. If the characteristics imaging criteria for hepatocellular carcinoma are fulfilled, then a confirmatory biopsy is not needed.
- If imaging criteria are not fulfilled, then a USG guided or a CT guided biopsy of the liver lesion must be performed for diagnosis.
- A PET-CT Scan must be performed following the diagnosis, to see the extent of spread of the liver cancer.
Liver Cancer Survival rate
- Hepatocellular carcinoma is an extremely aggressive cancer with high rates of recurrence.
- In the advanced stages, a cure is not possible. With current therapies, the disease can only be controlled. The treatment then remains palliative.
- In the initial stages, with surgery, recurrence rates are lower and a cure may be possible.
Liver Cancer Treatment
If the cancer in the liver is a secondary spread from another cancer elsewhere in the body, the treatment will follow the guidelines for the primary cancer.
Hepatocellular Cancer or Treatment of Primary Liver Cancer:
1. If there is a solitary cancer lesion within the liver, with no spread within the liver or outside the liver, there is no vascular invasion, and the liver function is normal, then a radical surgery is the treatment of choice. A part of the liver with the cancer is then removed. This is called a partial hepatectomy.
2. If the cancer cannot be treated with a surgical resection, due to spread within the liver, or due to underlying liver dysfunction, can opt for a liver transplantation, if a suitable donor can be found. There should be no spread of the cancer outside the liver if a transplant is being considered.
3. If a liver transplant is not possible, there is no spread of the cancer outside the liver, major blood vessels supplying the liver have not been invaded by the cancer, and the tumour spread within the liver is limited, then loco-regional liver directed therapies can be attempted.
Options include TACE- Trans-arterial chemoembolization, radiofrequency ablation, TARE-Trans arterial radio-embolisation, stereotactic body radiation, external beam radiation, HAIC- Hepatic arterial infusional chemotherapy. The choice of therapy depends on the size and number of the cancer deposits within the liver, the underlying liver function, presence or absence of cirrhosis and status of the blood vessels supplying the liver.
4. If there is extensive spread of the cancer within the liver, and/or spread outside the liver into other organs, or involvement by the cancer of major blood vessels supplying the liver, then systemic therapy is the best option. A combination of a targeted therapy plus immunotherapy is recommended as first line therapy. Drugs used are Bevacizumab with Atezolizumab.
5. If a targeted therapy is contraindicated, then a combination of immunotherapy drugs like Durvalumab plus Tremelimumab can be used. Nivolumab plus Ipilimumab is another combination showing good preliminary results.
6. Following progression on above regimens oral targeted therapy can be used in the second line regimens. Drugs that can be administered are Lenvatinib or Sorafenib. These tablets may also be used as first line therapy if the intravenous therapies are not accessible.
7. Other immunotherapy agents like Pembrolizumab can be used in the third line. Tablets like Cabozantinib and Regorafenib are also an option. Ramucirumab is a targeted therapy that can block the blood supply of the tumours and is a viable third line option.
8. Chemotherapy is largely ineffective in these cancers, regimens like GEMOX can be used but are not recommended.
Frequently Asked Questions For Liver Cancer
Without treatment, liver cancer spreads quickly and is eventually fatal within a few months to a year.
The possibility of cure depends on the stage the cancer is detected in. if diagnosed in the early stage and treated promptly a cure is possible.
Loss of appetite, weight loss, fatigue, right sided abdominal pain, jaundice, ascites are all warning signs of liver cancer.
Heavy alcohol intake leading to cirrhosis, is the main cause of liver cancer.
Liver cancer can arise at virtually any age if the predisposing factors like heavy alcohol consumption or chronic liver disease leading to cirrhosis are present.
Yes, liver cancer is aggressive and spreads rapidly.
In the initial stages, the liver cancer may remain asymptomatic. There may be vague symptoms like loss of appetite, weight loss and weakness. In the final stages, signs of liver failure are seen, like an abdominal mass, jaundice, ascites, breathlessness, bleeding tendency, haematemesis and melaena.
The treatment for liver cancer depends on the stage it is detected in and the extent of spread of the cancer. In the early stage, surgery is an option. In the advanced stages oral targeted therapy and Immunotherapy are the best options.
Diagnosis is made by performing a dynamic contrast enhanced CT Scan or MRI of the liver along with an alpha fetoprotein level. If the characteristic imaging for a liver cancer is visualised, then a confirmatory biopsy is not needed.
Liver cancer can be suspected on performing a blood test to see the alpha fetoprotein level. Its elevation, particularly above 400ng/ml points to the diagnosis of a liver cancer.
Take action against liver cancer today - get screened and consult with Dr. Sujata Vasani
Renal Cancer Causes
- Smoking, tobacco use, and nicotine exposure are prime risk factors for renal cancer
- Hypertension seems to predispose to renal cancer occurrence though the precise reason for this is unknown.
- Obesity is another risk factor.
- Chronic kidney disease with polycystic kidney disease is linked to renal cancer.
- Exposure to asbestos, cadmium, and petroleum by-products are risk factors.
- Heavy and prolonged use of drugs like aspirin, diclofenac, and other NSAIDS are linked to kidney cancer.
- Chronic hepatitis C infection, sickle cell disease, and previous history of radiation to the kidney given during treatment for childhood cancer, all increase the risk.
- Some renal cancers can be hereditary in nature, linked to underlying mutations. Having a first-degree relative with renal cancer increases the risk as well. Inherited syndromes passed on from one generation to the next also predispose to renal cancer. An example is hereditary papillary renal carcinoma.
Renal Cancer Symptoms & Signs
- A large number of patients may remain asymptomatic until the cancer has increased in size.
- Renal cancer may be discovered incidentally on sonography done for another purpose or as a routine health check.
- Symptoms usually arise when the cancer has started spreading and invading the surrounding tissues.
- Abdominal pain, either localized to one of the flanks, in the region of the involved kidney, or generalized in nature can occur.
- A scrotal varicocele can occur, usually on the left side, in males. This is due to obstruction of the gonadal venous drainage by renal cancer.
- Loss of appetite, weight loss, fatigue, and weakness are seen as renal cancer progresses.
- As cancer spreads into distant organs and invades major blood vessels, lower limb swelling, ascites, blood clots in major blood vessels, underlying liver dysfunction, and lung metastases causing cough and breathlessness can all occur.
- Paraneoplastic symptoms like anemia can develop. Often this can be seen several months before the actual diagnosis of renal cancer.
- Similarly, a few patients can develop intermittent fever associated with loss of appetite, weight loss, night sweats, and weakness.
- Hypercalcemia can occur as a part of the paraneoplastic syndrome or due to extensive bony metastases.
- Hematuria or bleeding in the urine can be seen due to the renal cancer invading the collecting system. It can become severe as the cancer progresses; the passage of blood clots may then be seen with the urine.
- These can lead to colicky abdominal pain and can be associated with significant distress and discomfort.
- An abdominal or flank mass may be felt as cancer increases in size. It would feel firm, would move with respiration, and would be better felt in a thin individual.
Treatment of Renal Cancer
Patients who are diagnosed in the early stages, before development of metastases, when the cancer is still localised within the kidney or has extended only into the immediate surrounding tissues, can undergo a curative surgery.
If the cancer is small, then a partial nephrectomy can be performed, meaning only a part of the kidney with the cancer has to be removed.
If the cancer is large, or has invaded the blood vessels and the surrounding tissues, then a radical nephrectomy is required. This involves removal of the entire kidney with the draining lymph nodes.
Renal cancers at a high risk of recurrence even after a complete surgery, have the option of receiving adjuvant immunotherapy with Pembrolizumab for a year. This treatment has been found to greatly reduce the risk of recurrence and improve chances of a cure.
If the renal cancer is detected in the advanced stage, when it has metastasised to other organs like the adrenal glands, liver, lungs, bones or brain, then a curative surgery is not possible. With treatment this cancer can be controlled but not cured.
Systemic treatment is required for such patients, diagnosed with stage 4 renal cancer.
A combination of targeted therapy and immunotherapy is recommended as a first line regimen. Two immunotherapy agents with differing but synergistic mechanisms of action may also be used upfront.
Options are Axitinib with Pembrolizumab, Lenvatinib with Pembrolizumab or Nivolumab with Ipilimumab.
Oral targeted therapy that includes the anti-angiogenic or VEGF inhibitors and the mTOR pathway inhibitors can be used as second line therapy or upfront in patients who cannot receive immunotherapy.
Oral targeted therapy that can be used is Sunitinib, Pazopanib, Cabozantinib, Lenvatinib or Axitinib.
Everolimus is the mTOR inhibitor that can be given orally.
If oral therapy is utilised initially, immunotherapy can be used in the second line on disease progression.
Frequently Asked Questions For Renal Cancer
Renal cancer can be completely cured with appropriate treatment if detected in the initial stages.
Yes, renal cancer can become serious if left untreated. It can spread rapidly eventually proving fatal.
Abdominal pain, an abdominal mass and hematuria or bleeding in the urine are the primary symptoms of renal cancer.
Renal cancer originates in one of the kidneys.
Abdominal pain, hematuria and an abdominal mass are considered the 3 primary signs of renal cancer.
Clear Cell Carcinoma is the commonest type of kidney cancer.
If detected in the initial stages and treated promptly, kidney cancer has an excellent survival rate.
Yes, alcohol intake is associated with an elevated risk of renal cancer.
Kidney cancer may be detected incidentally when a sonography is performed for another reason, or it may be diagnosed when a sonography is performed to evaluate symptoms of hematuria or abdominal pain. A biopsy of a mass detected on sonography gives the diagnosis.
Renal cancer usually occurs between the age of 60 to 80. It is unusual before the age of 40.
Consult with Dr. Sujata Vasani for possible renal cancer if you experience persistent lower back pain, blood in the urine, or unexplained weight loss
Vaginal and Vulvar Cancer
Vulvar cancer is one of the less common gynaecologic malignancies. Human papillomavirus infection is associated with the majority of vulvar cancers. This cancer is usually seen in elderly women, in their 60s and 7os. It is usually detected in the early stages and carries a reasonably good prognosis. Squamous cell carcinoma of the vulva is the pathology usually seen. A prior history of cervical cancer, tobacco and nicotine exposure, smoking, reduced immunity, and vulvar and cervical intraepithelial neoplasia are all risk factors for this cancer.
Symptoms and Signs
- A large number of patients are asymptomatic on presentation. A vulvar lesion in the form of an ulcer, a mass or a plaque is usually felt by the patient.
- Patients may present with bleeding from the vulvar region or complain of itching. Occasionally, the draining lymph nodes may be involved and palpable.
Vaginal and Vulvar Cancer Treatment
Localised Cancer
If the vulvar cancer is localised then a curative surgery can be performed. A radical excision must be performed. Large lesions would require a modified radical vulvectomy.
Cancers at a high risk of recurrence post-surgery, due to a size above 4cm or due to close or positive margins, or if the regional lymph nodes are invaded by the cancer, then these patients also require post operative radiation.
In case multiple lymph nodes are found to be involved with the cancer, then adjuvant chemotherapy is also required with radiation.
Locally advanced cancer
These patients may be surgically inoperable due to the cancer spreading into the surrounding tissues and lymph nodes.
Concurrent chemotherapy with radiation administered to the vulva, lymph nodes and surrounding tissues is the treatment of choice. Weekly cisplatin is given with daily radiation.
A few patients may achieve complete disease control with the above treatment. Those who experience a partial response can undergo a surgery to resect the residual disease.
Metastatic cancer
In case the cancer has already spread to multiple organs, then chemotherapy remains the best option.
Paclitaxel and carboplatin are the chemotherapy drugs recommended.
Vaginal and Vulvar Cancer Prevention
- A majority of both vaginal and vulvar cancers are associated with human papilloma virus infection.
- Smoking, tobacco consumption, nicotine exposure, are other well known risk factors.
- Reduced immunity is another risk factor.
- Regular, yearly health checks along with regular sonographies are recommended for early cancer detection.
- The HPV vaccine that provides protection against multiple human papilloma virus genotypes is the best method to protect against HPV infection and the subsequent development of cancer.
- Avoidance of smoking, tobacco and alcohol are the other options to reduce the cancer risk.
Human Papilloma Virus (HPV) In Men
- Men can also be infected with the human papilloma virus. There are various infections which can occur, benign and cancerous.
- Cutaneous warts, plantar and flat warts are skin infections, they are spread through touch and skin to skin contact. Both men and women can be infected.
- Genital warts are caused by HPV types 6 and 11. Sexual contact with an infected individual is believed to be the mode of spread.
- Immunocompromised men, especially those with HIV, men with another male as a sexual partner are particularly vulnerable to developing an HPV related cancer.
- Anal cancer is particularly seen in these individuals.
- Penile cancer can be HPV associated as well.
- Squamous cell cancer of the head and neck shows a strong association with HPV, especially HPV type 16. Cancers of the oropharynx, of the tonsil and of the tongue are generally seen with HPV infection. The mode of spread is sexual contact, especially when it is between two males, and is linked with high risk sexual behaviour.
- Vaccination against HPV infection in males provides excellent protection. It especially reduces the risk of developing an HPV related malignancy.
- HPV prevalence in males can be as high as 73%. The risk factors for contracting HPV is high risk sexual activity, multiple partners, an immunocompromised status, HIV infection, lack of condom usage during intercourse, the circumcision status, prior history of a sexually transmitted infection which increases risk for HPV and homosexual status.
- Circumcision is believed to reduce the risk of contracting HIV.
- Heterosexual men can also contract HPV, although their risk is believed to be lower.
Frequently Asked Questions For Vaginal and Vulvar Cancer
Vulvar cancer usually presents as a plaque like lesion, a mass or an ulcer involving the vulva. Patients may remain asymptomatic or present with bleeding from the vaginal area or itching.
The first stage is a localized lesion involving only the vulvar region with no spread elsewhere. A plaque, an ulcer, or a mass involving the vulva may be seen or felt.
Initial spread of the cancer occurs to the superficial inguinal lymph nodes which are the regional draining lymph nodes.
Vulvar cancer can develop and spread rapidly without appropriate treatment, over a period of a few months.
Human papilloma virus infection is the commonest cause of vulvar cancer. Chronic inflammation of the vulva is a less common risk factor.
Radical concurrent chemotherapy and radiation in curative doses can be offered to patients who are not able to undergo a curative surgery.
Yes, if not treated promptly and appropriately, vulvar cancer is a serious disease. It can spread rapidly and prove fatal eventually.
Yes, vulvar cancer can be cured if detected and treated in the initial stages.
Vulvar cancer in the early stages carries a favourable prognosis with an extremely good prognosis if treated promptly.
The duration of treatment depends on the stage the cancer is detected in. If surgery and chemoradiation are required treatment would usually require about 6 months for completion.
Surgery followed by radiation or curative, concurrent chemoradiation are the treatments recommended depending on the stage the cancer is detected in.
Locally advanced vulvar cancer can be cured with concurrent chemoradiation. If it has metastasised to distant organs, then a cure is not possible. The cancer then can only be controlled.
Learn more about early detection and treatment options for Vaginal and Vulvar Cancer at our clinic
Cervical Cancer Causes: HPV, Sex, and Other Risks
- Human Papilloma Virus infection is responsible for the majority of cervical cancers seen in women.
Risk factors for HPV related cervical cancers are: - An earlier age of onset of sexual activity increases the risk, especially if it begins at 18 years of age or earlier.
- Multiple sexual partners, especially if more than 2 partners increases the risk.
- A sexual partner who has had multiple other partners, who has a prior history of HPV or other sexually transmitted diseases, increases the risk of developing an HPV related cervical cancer.
- A personal history of sexually transmitted diseases like gonorrhoea and chlamydia is a high risk for cervical cancer development.
- An early pregnancy, occurring before 20 years of age, having multiple full-term births- 3 or more are both considered risk factors.
- An immunosuppressed status, especially HIV infection is a risk factor.
- A prior history of vulvar or vaginal cancer or intraepithelial neoplasia are also risk factors, as these are also usually caused by the HPV infection.
- Non-HPV related causes that can cause cervical cancer are long term oral contraceptive use, history of smoking and tobacco use and heavy alcohol consumption.
- Some of the cervical cancers have a hereditary basis, with a positive family history increasing the risk for its occurrence.
Stages of Cervical Cancer
There are basically three main stages of cervical cancer -
Localized cervical cancer:
This is the initial or early stage of cervical cancer. In this stage, the cancer is localized within the cervix. There is no spread of the cancer. A patient in this stage can be cured completely, either by undergoing a radical surgery or non-surgically, by receiving concurrent radical radiotherapy with weekly chemotherapy. Cisplatin is the drug used for chemotherapy.
Locoregionally advanced cervical cancer:
- In this stage, the cervical cancer has invaded the surrounding tissues and has extended outside the cervix. The regional lymph nodes may be involved.
- However, there is no spread to the distant organs like the liver and lungs. Patients in this stage have chances of a cure depending on the extent of regional spread.
- Such cancers must first be treated using neoadjuvant chemotherapy. Paclitaxel and Cisplatin are the drugs used. 2 to 3 cycles must be administered.
- This can be followed by a regimen that utilizes curative concurrent radiotherapy in combination with weekly chemotherapy using Cisplatin.
Metastatic or stage 4 cervical cancer:
- In this stage, the cervical cancer has metastasised extensively with spread to the lungs, liver, bones, lymph nodes etc.
There is no role of surgery. In this stage, a cure is not possible. With medication, the cancer can be controlled. The treatment aim is palliation and maintaining the patient’s quality of life. - Chemotherapy in combination with immunotherapy and targeted therapy form the treatment protocol.
Paclitaxel and Carboplatin are the chemotherapy drugs of choice. - A detailed molecular profiling must be performed on the cervical cancer specimen to determine which targeted therapy can be given, depending on the disease-causing mutations detected. Markers for immunotherapy must be analyzed as well to assess the degree of benefit it will provide.
Cervical Cancer in India and HPV Vaccination
- Cervical cancer burden in India has been increasing exponentially over the past decade.
- A lack of awareness, poverty, lower socio-economic status and poor literacy rates are all contributory factors.
- As a result, few women receive timely treatment for this otherwise curable malignancy. The majority are diagnosed in the advanced stages, by when treatment administered can only be palliative.
- However, the discovery that the human papilloma virus is responsible for 90% of the cervical cancers has resulted in implementation of preventive strategies against cervical cancer, via efforts preventing the contraction of HPV.
- Cervical cancer screening strategies have been put in place and are being practiced widely.
- The advent of effective HPV vaccination has contributed immensely to the above efforts.
- Along with cervical cancer screening, this should enable a reduction in the cervical cancer load, detection at earlier stages, which in turn will enable multiple lives to be saved.
HPV Vaccination
- Is an effective preventive strategy against cervical cancer, providing 99% protection against the majority of the disease causing HPV strains.
- In addition, protection is also provided against other cancers caused by HPV, like anal cancer, oropharyngeal cancer, vulvar & vaginal cancers (in women), penile cancer in men and anogenital warts. Both men and women must receive the HPV vaccine.
- The recommended age is before the onset of sexual activity in both sexes. The ideal age is 11-12 years. However, vaccination can begin at 9 years of age.
- Adolescents 13 years and above, and adults up to 45 years of age who have never been sexually active must receive the vaccine as well.
- Health care workers must receive the vaccination if they have a risk of HPV exposure due to their vocation, like family physicians, gynaecologists and dermatologists.
- HPV in vapours generated during surgical excision of lesions can lead to an infection as well.
- Once the individual is sexually active, HPV exposure and infection occurs during sexual intercourse.
- Vaccination after exposure does not provide effective protection against the cancers. The more the number of sexual partners, the higher the risk of infection.
Currently, there are 3 principal HPV vaccines available
- The human papilloma virus quadrivalent vaccine, known as Gardasil, that provides protection against HPV types 6, 11, 16 & 18.
- The human papilloma virus 9-valent vaccine, known as Gardasil 9, that provides protection against HPV types 6, 11, 16, 18, 31, 33, 45, 52 & 58.
- The human papilloma virus bivalent vaccine, known as Cervarix, that provides protection against HPV types 16 & 18.
- The Gardasil 9 vaccine is the vaccine of choice as it provides the maximum protection against HPV, by targeting 9 HPV cancer causing strains.
Vaccination schedule
- If administered before 15 years, 2 doses must be given, 6 months apart.
- If administered at 15 years or older, 3 doses must be given, at 0, 1 to 2 months and 6 months.
- Immunocompromised patients must receive 3 vaccine doses in the above schedule.
- It must be remembered that the HPV vaccine is not a treatment for an established HPV infection, cervical cancer, anal cancer or any other HPV associated malignancy.
Frequently Asked Questions For Cervical Cancer
In the initial stages, cervical cancer remains asymptomatic. Symptoms may be seen as the cancer progresses. These are usually irregular or heavy bleeding per vaginum, occurring as a part of the menstrual cycle or between periods. Post intercourse bleeding may also be seen.
Cervical cancer should be suspected in case of unusually heavy bleeding during periods, irregular vaginal bleeding, bleeding in between periods, post intercourse bleeding, a foul smelling, watery or a mucoid discharge per vaginum, pelvic pain, pain involving the lower back, an ulcerated or a bleeding lesion detected on examination over the cervix, bleeding during urination or passage of fresh blood with stools.
Human Papilloma Virus infection is the main cause of cervical cancer.
Yes, cervical cancer is a serious disease. Without appropriate treatment, it can prove fatal.
The Pap smear or cervical cytology test and tests for detection of cervical cancer-causing HPV types are the 2 most important screening studies.
Cervical cancer risk usually increases after the age of 50.
Cervical cancer can spread rapidly if left untreated, and can eventually prove fatal.
Between 11-12 years is the ideal age for HPV vaccination. But vaccination can be started at 9 years of age as well. This is applicable for boys and girls. It may be given up to 45 years of age in women who have not had sexual intercourse. The same applies to males.
Men usually contract HPV on homosexual contact with another male partner. Anal sex is a significant risk factor. Immunocompromised men, especially those with HIV are particularly vulnerable. However, intercourse with an HPV infected female partner can also result in the male partner contracting the infection. Multiple sexual partners increase the risk.
Most HPV infections in males will resolve spontaneously, usually within 12 months. A reduction in the host immunity results in the HPV infection producing symptoms and progressing to cancer in some individuals. An HIV infected person is a prime example.
Yes, there are currently 3 vaccines available for cervical cancer.
There are 3 vaccines for cervical cancer available in India. These are the Cervarix, Gardasil and Gardasil-9 vaccines. An Indian cervical cancer vaccine is expected to be launched in 2023, it is indigenously prepared and is called Cervavac.
Don't delay, schedule your cervical cancer screening today to prioritize your reproductive health
Ovarian Cancer
Ovarian cancer is often treated with a combination of surgery, chemotherapy, and other treatments.
Lung Cancer
Lung cancer treatment plans may include surgery, chemotherapy, radiation therapy, targeted therapy, immunotherapy, or clinical trials.
Blood Cancer
Treatment for blood cancers such as leukemia, lymphoma, and myeloma often involves chemotherapy, radiation therapy, and/or targeted therapies.
Get your Treatment Plan
Do you know what kind of cancer treatment might work best for you? Learn the fundamentals from Dr. Sujata about some of the most frequent treatments.